The concept of chronic disease management within community settings has gained significant traction in recent years as healthcare systems worldwide grapple with the rising burden of non-communicable diseases. Unlike traditional hospital-centric models, community-based approaches emphasize localized care, patient empowerment, and long-term sustainability. These models recognize that managing conditions like diabetes, hypertension, and cardiovascular diseases requires more than episodic clinical interventions—it demands continuous engagement within the environments where people live and work.
At the heart of this paradigm shift is the understanding that chronic illnesses are not merely biomedical issues but deeply intertwined with social determinants of health. Factors such as income levels, education, access to nutritious food, and social support networks play pivotal roles in disease progression. Community models leverage this insight by integrating healthcare services with existing social structures, creating ecosystems where patients receive holistic support. For instance, local health workers might collaborate with neighborhood grocery stores to promote healthy eating or organize walking groups to encourage physical activity.
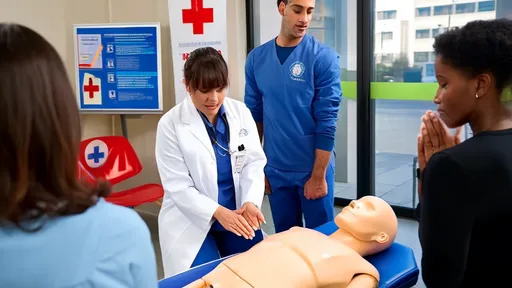
One particularly innovative aspect of community-based chronic disease management involves the strategic use of lay health educators. These individuals, often drawn from the communities they serve, undergo specialized training to provide basic health monitoring, education, and motivational support. Their strength lies in cultural competence and the ability to build trust—qualities that sometimes elude even the most skilled medical professionals working outside their native contexts. Studies have shown that such peer-led initiatives can dramatically improve medication adherence and lifestyle modification rates, particularly in underserved populations.
The digital revolution has further amplified the potential of community models through telehealth and remote monitoring technologies. Mobile health applications now enable patients to track vital signs, receive medication reminders, and consult with healthcare providers without leaving their neighborhoods. This technological layer complements rather than replaces the human element of community care, creating hybrid models that combine the efficiency of digital tools with the warmth of face-to-face interactions. In rural areas especially, these innovations have bridged critical gaps in specialist access while maintaining the community's central role in ongoing disease management.
Financial sustainability remains a pressing challenge for many community-based programs. Unlike acute care services that generate immediate revenue streams, the economic benefits of chronic disease prevention and management manifest over extended periods. Forward-thinking health systems are experimenting with value-based payment structures that reward providers for long-term health outcomes rather than service volume. Some communities have established innovative partnerships with local businesses and insurers, creating shared investment models where improved population health translates to economic gains for multiple stakeholders.
The psychological dimension of chronic illness management in community settings deserves particular emphasis. Living with a persistent health condition often leads to emotional distress that clinical settings frequently overlook. Community models address this through support groups, counseling services, and wellness activities that nurture mental resilience. The familiar environment of neighborhood centers or local clinics tends to feel less intimidating than hospitals, encouraging more consistent participation in self-care activities. This aspect proves especially valuable for elderly patients or those managing multiple chronic conditions simultaneously.
Evaluation methodologies for community-based chronic disease programs require distinct approaches compared to conventional clinical trials. Traditional metrics like hospitalization rates and biomarker improvements remain important, but equally crucial are measurements of community engagement, quality-of-life enhancements, and social connectedness. Mixed-method assessments that combine quantitative data with patient narratives often provide the most comprehensive picture of program effectiveness. Such evaluations frequently reveal unexpected benefits, like reduced social isolation among participants or improved health literacy spreading through family networks.
As urbanization accelerates globally, the community model of chronic disease management faces both challenges and opportunities. Dense urban environments can complicate the creation of tight-knit support networks, yet they also concentrate resources and talent that can be mobilized for population health initiatives. Some cities have begun redesigning physical spaces to support healthier lifestyles—creating pedestrian-friendly zones, community gardens, and accessible recreation facilities that passively encourage disease-preventing behaviors. These urban planning considerations represent the next frontier in environmental approaches to chronic disease control.
The future trajectory of community-based chronic disease management will likely see increased personalization through advances in genomics and precision medicine. Imagine neighborhood health centers equipped to provide tailored lifestyle recommendations based on genetic risk profiles, or community exercise programs designed around prevalent metabolic characteristics in the local population. Such innovations could make prevention and management strategies even more relevant to specific communities while maintaining the inclusive, accessible nature that defines this care model.
Ultimately, the success of community approaches to chronic disease hinges on viewing health not as the absence of illness but as the presence of supportive ecosystems. This philosophy recognizes that lasting well-being emerges from daily interactions with one's environment, social circles, and local institutions. As healthcare systems worldwide confront the unsustainable costs of reactive medicine, the community model offers a path forward that is both clinically effective and fundamentally human in its execution.
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025