The evaluation of healthcare quality has become a cornerstone in modern medical systems, shaping policies, patient outcomes, and institutional accountability. As healthcare systems worldwide strive for excellence, the development and implementation of robust healthcare quality evaluation indicator systems have gained prominence. These frameworks serve as vital tools for measuring performance, identifying gaps, and driving continuous improvement in patient care.
In recent years, the focus on healthcare quality has intensified, with stakeholders demanding transparency and measurable outcomes. The shift from volume-based to value-based care has further underscored the need for comprehensive evaluation mechanisms. Hospitals, clinics, and public health organizations now rely on sophisticated quality metrics to benchmark their services against national and international standards. This paradigm shift reflects a broader recognition that quality measurement is not merely an administrative exercise but a fundamental component of patient-centered care.
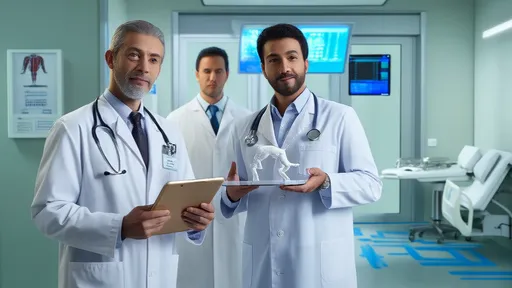
The complexity of healthcare delivery necessitates a multidimensional approach to quality assessment. Traditional indicators such as mortality rates and infection control remain critical, but contemporary frameworks incorporate a wider array of parameters. Patient satisfaction, accessibility of care, and the efficiency of clinical workflows now feature prominently in evaluation systems. This evolution mirrors the growing understanding that healthcare quality extends beyond clinical outcomes to encompass the entire patient experience.
One of the most significant challenges in healthcare quality evaluation lies in balancing standardization with contextual relevance. While international benchmarks provide valuable reference points, local factors such as resource availability and population health needs must inform indicator selection. Policymakers and healthcare leaders increasingly emphasize the importance of adaptable frameworks that can accommodate regional variations without compromising comparability. This delicate equilibrium ensures that quality improvement efforts remain both meaningful and measurable across diverse settings.
The integration of technology into quality measurement has opened new frontiers in healthcare evaluation. Electronic health records, real-time data analytics, and artificial intelligence applications enable more dynamic and precise monitoring of quality indicators. These technological advancements facilitate not just retrospective analysis but also predictive modeling, allowing healthcare providers to anticipate and address potential quality issues before they escalate. The marriage of digital innovation and quality measurement represents a transformative leap in how healthcare performance is assessed and enhanced.
Patient-reported outcomes have emerged as a crucial dimension of contemporary quality evaluation systems. Moving beyond clinical metrics, these indicators capture the patient's perspective on treatment effectiveness, symptom burden, and quality of life improvements. This patient-centric approach acknowledges that healthcare quality ultimately resides in the lived experience of those receiving care. As value-based payment models gain traction, such patient-focused metrics are becoming increasingly influential in determining reimbursement and institutional rankings.
The implementation of healthcare quality indicators frequently encounters operational challenges, particularly in resource-constrained settings. Data collection burdens, staff training requirements, and infrastructure limitations can hinder effective quality monitoring, especially in developing healthcare systems. Addressing these barriers requires strategic investments in health information systems, capacity building, and the development of simplified yet meaningful indicator sets tailored to local contexts.
Looking ahead, the future of healthcare quality evaluation will likely see greater emphasis on outcome measures rather than process indicators. While tracking compliance with clinical protocols remains important, the ultimate test of healthcare quality lies in its impact on patient health status and wellbeing. This outcomes-focused approach aligns with the broader movement toward precision medicine and personalized care, where treatment effectiveness is judged by its actual results in specific patient populations.
The globalization of healthcare quality standards presents both opportunities and challenges. International accreditation bodies and cross-border quality comparisons drive improvement through competition and knowledge sharing. However, the uncritical adoption of foreign quality indicators without local validation risks creating measurement systems that are technically sophisticated but clinically irrelevant. The most effective quality frameworks will be those that synthesize global best practices with localized adaptations.
As healthcare systems continue to evolve, so too must their approaches to quality evaluation. The next generation of quality indicators will need to address emerging priorities such as health equity, environmental sustainability, and the integration of mental health services. These expanding dimensions reflect the growing recognition that high-quality healthcare must respond not just to individual patient needs but to broader societal challenges as well. The ongoing refinement of quality measurement tools ensures they remain relevant in an ever-changing healthcare landscape.
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025