The evolution of medical robotics has ushered in a new era of precision, efficiency, and safety in healthcare. These sophisticated machines are no longer confined to the realms of science fiction but have become indispensable tools in modern medicine. As the technology matures, it has become increasingly important to classify medical robots based on their technical capabilities, applications, and levels of autonomy. Understanding these gradations is critical for healthcare providers, policymakers, and manufacturers alike, as it informs decision-making regarding adoption, regulation, and further innovation.
The foundation of medical robotics lies in their ability to augment human capabilities. At the most basic level, we encounter robots designed for repetitive tasks or those requiring superhuman precision. These systems often operate under direct human control, with surgeons or technicians guiding their every move. For instance, robotic arms used in laboratories for sample handling exemplify this category. While they lack autonomous decision-making, their value lies in eliminating human error in monotonous or highly precise operations. Such devices have become commonplace in diagnostic labs and pharmaceutical research facilities, where consistency is paramount.
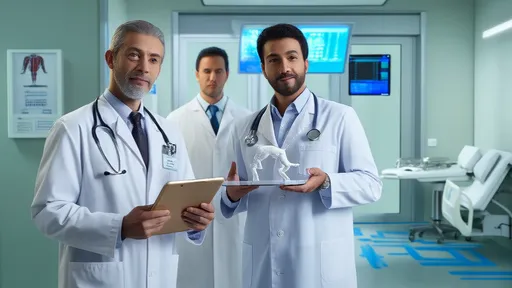
Moving up the technical hierarchy, we find semi-autonomous systems that blend human oversight with machine intelligence. These robots can perform certain predefined sequences independently once initiated by a human operator. Surgical assistants in operating rooms represent this tier perfectly. They can suture with perfect stitch length or maintain tremor-free positioning for extended periods, tasks that would fatigue even the steadiest human hands. The da Vinci Surgical System, perhaps the most recognizable name in medical robotics, operates at this level - enhancing a surgeon's capabilities while never acting without explicit human direction.
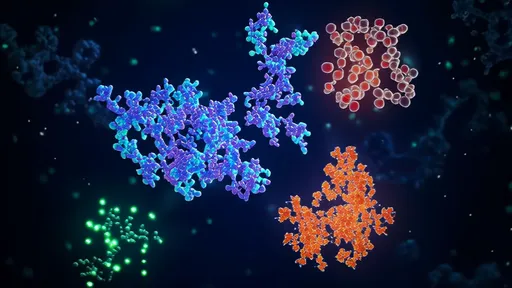
The frontier of medical robotics belongs to highly autonomous systems capable of complex decision-making. These advanced machines incorporate artificial intelligence, machine learning, and real-time data processing to perform tasks with minimal human intervention. Autonomous diagnostic robots that can analyze medical images and detect abnormalities with accuracy rivaling or surpassing human radiologists represent this cutting-edge category. Some experimental systems are even exploring autonomous robotic surgeons that could perform certain procedures start-to-finish, though ethical and regulatory hurdles remain significant barriers to widespread adoption of such technology.
Beyond physical robots that interact with patients or medical instruments, another dimension of medical robotics exists in virtual systems. These include AI-powered diagnostic tools, treatment planning algorithms, and predictive analytics platforms. While they lack a physical form, their impact on medical decision-making qualifies them as part of the robotic ecosystem. The most advanced virtual systems can process vast amounts of patient data, compare it against global medical knowledge bases, and suggest treatment options with supporting evidence - all in real time during patient consultations.
Technical classification of medical robots also considers their intended environment and risk profile. Robots designed for non-invasive diagnostics occupy a different tier than those performing invasive surgical procedures. Similarly, systems intended for use in controlled operating rooms undergo more stringent evaluation than those assisting with rehabilitation in clinical settings. This environmental consideration adds another layer to the technical grading system, ensuring that safety protocols match both the robot's capabilities and its operational context.
The integration of haptic feedback represents another important differentiator in medical robot classification. Basic systems may provide visual guidance alone, while advanced platforms incorporate tactile feedback that allows human operators to "feel" through the robot. This technology is particularly crucial in delicate surgical applications where tissue resistance and texture provide important information to the surgeon. The presence and sophistication of such feedback mechanisms significantly influence where a robotic system falls in the technical hierarchy.
Connectivity and data integration capabilities have emerged as crucial classification factors in the era of smart hospitals. Standalone robotic systems are increasingly giving way to networked devices that share information with electronic health records, imaging systems, and other hospital infrastructure. The most advanced medical robots can not only perform their primary function but also contribute to a continuous learning ecosystem, improving their performance over time based on aggregated data from thousands of procedures across multiple institutions.
As we look toward the future, the boundaries between these technical grades continue to blur. Machine learning algorithms initially developed for autonomous systems are finding their way into semi-autonomous platforms, enhancing their capabilities. Similarly, safety features from highly regulated surgical robots are being adapted for use in less critical applications. This cross-pollination of technologies accelerates overall progress while complicating clear-cut classification schemes. The medical community continues to debate whether classification should focus on technical specifications or clinical outcomes, with compelling arguments on both sides.
The regulatory landscape struggles to keep pace with these rapid advancements. Current classification systems, often based on risk assessment rather than technical sophistication, sometimes group disparate technologies together while separating similar ones. This creates challenges for both developers seeking approval and healthcare providers trying to compare options. International harmonization of medical robot classification remains an ongoing challenge, with different regions adopting varying approaches based on their healthcare systems and technological infrastructure.
Training requirements form another practical dimension of medical robot classification. Basic systems might require minimal operator training, while advanced platforms demand extensive certification programs. This human factor significantly impacts adoption rates and practical utility in clinical settings. Some institutions have developed proprietary classification systems based on training complexity, creating yet another lens through which to view the medical robotics landscape.
Economic considerations inevitably influence how medical robots are categorized and adopted. Higher technical grades typically command premium pricing, creating access disparities between well-resourced medical centers and smaller community hospitals. Some manufacturers have begun offering tiered product lines with varying capability levels at different price points, effectively creating commercial classifications that mirror technical ones. This commercialization of the classification system has both positive and negative implications for the field's development.
The patient perspective adds another layer of complexity to medical robot classification. While technical specifications matter to engineers and surgeons, patients often care more about outcomes, comfort, and perceived safety. Some studies suggest that patients attribute greater capability to robotic systems than they actually possess, based on appearance and marketing. This perception gap between technical reality and patient understanding represents an important consideration in how these technologies are deployed and discussed in clinical settings.
Looking ahead, the classification of medical robots will likely evolve alongside the technology itself. As artificial intelligence becomes more sophisticated and robotics more miniaturized, new categories will emerge that we can scarcely imagine today. The development of nanoscale medical robots, for instance, could create entirely new classification parameters based on size and mode of interaction with human biology. Similarly, the integration of quantum computing could revolutionize processing capabilities, necessitating new ways to categorize robotic intelligence.
The standardization of medical robot classification remains an ongoing challenge for the industry. Various professional organizations and standards bodies continue to work toward consensus frameworks that can accommodate both current technologies and future innovations. These efforts aim to create a common language that facilitates research, development, regulation, and clinical adoption - ultimately benefiting patients worldwide through safer, more effective robotic medical solutions.
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025