The interpretation of genomic data has become a cornerstone of modern biomedical research, clinical diagnostics, and personalized medicine. As sequencing technologies advance and costs decline, the volume of genomic information available to researchers and clinicians has grown exponentially. However, the sheer complexity of this data presents significant challenges in establishing standardized interpretation frameworks that ensure accuracy, consistency, and clinical relevance.
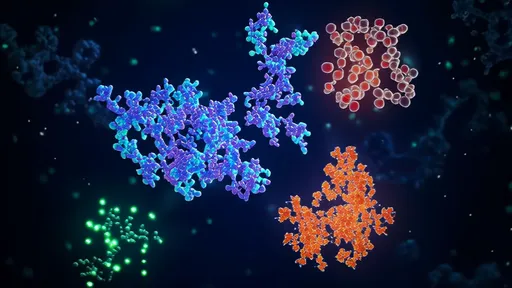
At the heart of genomic data interpretation lies the need to distinguish between benign variants and those with potential clinical significance. This process requires not only sophisticated computational tools but also a deep understanding of biological context. Variant classification systems, such as those developed by the American College of Medical Genetics and Genomics (ACMG), provide structured approaches to assessing pathogenicity. These guidelines consider multiple lines of evidence, including population frequency data, computational predictions, functional studies, and segregation analysis.
The clinical utility of genomic interpretations depends heavily on the quality of reference databases. Resources like gnomAD, ClinVar, and dbSNP serve as critical repositories for variant frequency and phenotypic associations. However, disparities in population representation across these databases can lead to interpretation biases, particularly for underrepresented ethnic groups. This limitation underscores the importance of ongoing efforts to diversify genomic datasets and improve the inclusivity of reference populations.
Functional validation remains an essential component of variant interpretation, despite the increasing reliance on computational predictions. Laboratory experiments that assess the impact of genetic variants on protein function or gene expression provide crucial evidence for classification. The integration of multi-omics data, including transcriptomics and proteomics, offers additional layers of biological context that can refine interpretation accuracy. This systems biology approach helps bridge the gap between genetic variation and phenotypic expression.
Emerging technologies like long-read sequencing are reshaping interpretation standards by providing more complete genomic context. These methods enable better detection of structural variants and resolution of complex genomic regions that were previously difficult to analyze. As these technologies mature, interpretation guidelines must evolve to incorporate new types of variants and their potential clinical implications. The field is moving toward more dynamic standards that can adapt to technological advancements while maintaining rigorous evidence requirements.
The ethical dimensions of genomic interpretation cannot be overlooked, particularly when dealing with incidental findings or variants of uncertain significance. Professional societies continue to grapple with questions about which findings should be reported to patients and how to communicate complex genetic information effectively. These considerations are especially pertinent in pediatric genomics and reproductive medicine, where interpretation decisions may have implications for entire families.
Standardization efforts face particular challenges in cancer genomics, where tumor heterogeneity and somatic mutation patterns add layers of complexity to interpretation. Tumor-normal paired sequencing has become standard practice for distinguishing somatic from germline variants, but the clinical significance of many cancer-associated variants remains uncertain. The development of cancer-specific interpretation guidelines and the aggregation of treatment response data across institutions are critical for advancing precision oncology.
Quality control measures represent another critical component of genomic interpretation standards. Laboratories must implement rigorous protocols for variant calling, annotation, and interpretation to ensure reproducibility across different platforms and institutions. Proficiency testing programs and laboratory accreditation requirements help maintain consistency in clinical genomic testing. The establishment of international consortia for data sharing and method harmonization further supports the development of robust interpretation standards.
The rapid pace of discovery in functional genomics continually reshapes our understanding of variant impact. Non-coding variants, once largely ignored in clinical interpretation, are now recognized for their potential regulatory effects. Similarly, the growing appreciation for polygenic risk scores necessitates new frameworks for interpreting the combined effects of multiple common variants. These developments challenge the traditional variant-by-variant approach to interpretation and demand more integrative analytical methods.
As genomic medicine becomes more widespread, the need for clinician education in genomic interpretation grows proportionally. Many healthcare providers lack the training to critically evaluate genomic reports or understand their limitations. This knowledge gap highlights the importance of clear reporting standards and the development of decision support tools that can help translate complex genomic findings into actionable clinical insights.
The future of genomic interpretation will likely involve greater automation through artificial intelligence and machine learning approaches. While these technologies promise to improve efficiency and consistency, they also introduce new challenges regarding transparency and validation. Interpretation standards must address how to incorporate computational predictions while maintaining human oversight and clinical judgment. The balance between automated analysis and expert review remains an active area of discussion in the field.
International collaboration will be essential for advancing genomic interpretation standards globally. Differences in healthcare systems, regulatory environments, and population genetics necessitate flexible yet harmonized approaches. Organizations like the Global Alliance for Genomics and Health are working to facilitate data sharing and standard development across borders, recognizing that the utility of genomic medicine depends on its applicability to diverse populations worldwide.
Ultimately, genomic interpretation standards must remain responsive to both scientific advances and clinical needs. As our understanding of the genome deepens and new therapeutic opportunities emerge, the frameworks for interpreting genetic data will continue to evolve. The challenge lies in maintaining rigorous standards while allowing sufficient flexibility to incorporate new knowledge and technologies that can improve patient care.
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025