The seamless transition between acute care and rehabilitation services remains one of the most critical yet often overlooked aspects of modern healthcare systems. As populations age and chronic conditions become more prevalent, the need for effective rehabilitation care coordination has never been greater. Yet despite its importance, many patients still fall through the cracks during this vulnerable period of recovery.
At the heart of this challenge lies the fundamental disconnect between hospital-based acute care and community-based rehabilitation services. When a stroke patient is discharged from neurology, or when a trauma survivor leaves orthopedic care, their journey toward functional recovery is only beginning. Yet too often, these transitions happen without proper communication between specialists, rehabilitation teams, and primary care providers. The consequences can be devastating - unnecessary complications, delayed recovery, and in some cases, permanent loss of function that might have been prevented.
The current landscape reveals troubling gaps in continuity of care. In many healthcare systems, rehabilitation is treated as an afterthought rather than an integral component of the treatment continuum. Referrals to rehabilitation specialists frequently come too late, if at all. Discharge summaries often fail to include crucial details about functional status or rehabilitation potential. Perhaps most alarmingly, many patients and their families receive inadequate education about what rehabilitation entails or how to access appropriate services after leaving the hospital.
Financial and structural barriers further complicate these transitions. Insurance limitations frequently dictate the duration and type of rehabilitation services available, rather than clinical need. In some cases, patients are forced to navigate complex authorization processes at precisely the time when they are least equipped to do so. The result is what rehabilitation specialists call "the black hole" of post-acute care - a period when patients disappear from the healthcare system's radar until they either recover sufficiently or deteriorate to the point of requiring rehospitalization.
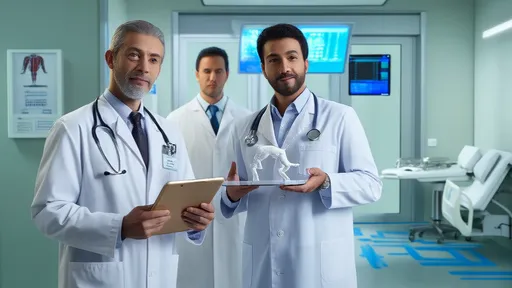
Emerging models of care coordination offer promising solutions to these systemic failures. Some leading medical centers have implemented "rehabilitation liaisons" - specialized clinicians who begin working with patients and families during the acute care phase to plan for rehabilitation needs. These transition specialists ensure that discharge plans include specific rehabilitation goals, follow-up timelines, and clear lines of communication between all providers involved in the patient's care.
Technology is playing an increasingly important role in bridging these gaps. Shared electronic health records that extend beyond hospital walls allow rehabilitation providers to access crucial information about a patient's hospital course, medications, and functional baselines. Tele-rehabilitation platforms enable specialists to monitor patients remotely and adjust treatment plans without requiring burdensome travel during the fragile post-discharge period. These digital tools are particularly valuable in rural areas where access to specialized rehabilitation services may be limited.
The most effective transition systems recognize that rehabilitation is not a single event but a process that evolves as the patient's needs change. A patient recovering from hip replacement surgery might progress from inpatient rehabilitation to outpatient physical therapy to community-based exercise programs over several months. At each stage, their care team should reassess goals and adjust the treatment plan accordingly. This requires not only clinical coordination but also mechanisms for tracking patient progress across different care settings.
Patient and family engagement represents another critical component of successful care transitions. Rehabilitation is fundamentally different from many other medical treatments in that its success depends heavily on the patient's active participation. Effective transition systems therefore include robust education components that help patients and caregivers understand their role in the recovery process. This might involve training family members in assistance techniques, providing clear instructions for home exercise programs, or connecting patients with peer support groups.
The economic argument for improving rehabilitation transitions is compelling. Studies consistently show that timely, appropriate rehabilitation reduces hospital readmissions, decreases long-term disability, and allows patients to return to work and independent living sooner. In an era of value-based healthcare, these outcomes translate to significant cost savings for health systems and payers alike. Yet despite this evidence, rehabilitation services remain chronically underfunded in many healthcare budgets.
Looking ahead, the rehabilitation field faces both challenges and opportunities. Workforce shortages in rehabilitation professions threaten to exacerbate existing gaps in care continuity. At the same time, advances in areas like regenerative medicine, neuroplasticity, and assistive technologies promise to expand what's possible in rehabilitation outcomes. What remains constant is the need for systems that can smoothly guide patients through each phase of their recovery journey.
Ultimately, the measure of a healthcare system's effectiveness shouldn't stop at saving lives - it must include restoring quality of life. Achieving this requires viewing rehabilitation not as an optional add-on, but as an essential component of comprehensive care. By strengthening the bridges between acute treatment and functional recovery, we can help patients not just survive their health challenges, but truly recover from them.
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025