The establishment of robust rare disease diagnosis and treatment networks has emerged as a critical priority in global healthcare systems. As nations grapple with the complexities of identifying and managing these often-overlooked conditions, collaborative frameworks are proving indispensable. These networks represent more than just medical infrastructure—they embody a fundamental shift in how societies address health inequities for vulnerable patient populations.
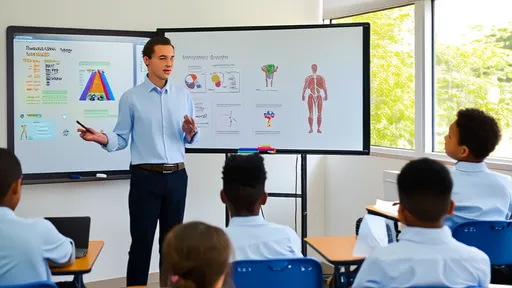
Rare diseases, though individually uncommon, collectively affect millions worldwide. The paradox lies in their prevalence—while each condition may impact a small percentage of the population, together they represent a significant public health challenge. Traditional healthcare models frequently fail these patients through delayed diagnoses, limited specialist access, and fragmented care pathways. This systemic neglect has spurred innovative approaches to network development that prioritize patient-centered solutions.
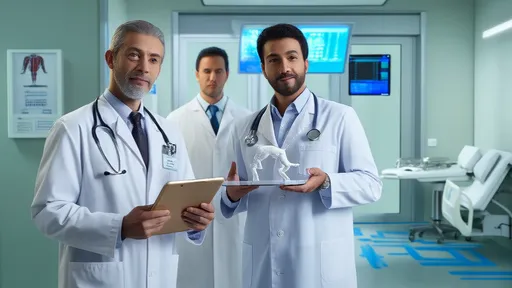
At the heart of effective networks lies multidisciplinary collaboration. Leading medical institutions are breaking down silos by creating interconnected teams spanning geneticists, pediatricians, neurologists, and other specialists. The Children's Hospital of Philadelphia recently demonstrated this approach through their integrated rare disease program, which reduced diagnostic odysseys from an average of 7 years to under 18 months for many conditions. Such successes highlight how coordinated expertise can transform outcomes.
Technological integration represents another cornerstone of network efficacy. Advanced telemedicine platforms now enable real-time consultations between rural clinicians and metropolitan specialists, while AI-assisted diagnostic tools help identify patterns across disparate symptoms. The European Reference Networks have pioneered this digital transformation, leveraging shared databases that aggregate clinical knowledge across 38 countries. These technological solutions don't replace human expertise—they amplify it.
Patient advocacy groups have become unexpected architects of network development. Organizations like the National Organization for Rare Disorders (NORD) have shifted from awareness campaigns to active participation in network design. Their "patient passport" initiative, which creates portable medical summaries for individuals with rare conditions, has been adopted by 23 U.S. states. This grassroots involvement ensures networks address real-world needs rather than theoretical models.
Financial sustainability remains the most persistent challenge. While startup funding often flows from government grants or philanthropic sources, long-term operation requires innovative financing models. Some networks have adopted value-based reimbursement structures, where payments align with measurable patient outcomes rather than service volume. Others explore cross-border funding pools, particularly for ultra-rare conditions requiring multinational collaboration.
The human impact of these networks manifests in unexpected ways. Beyond clinical metrics, quality-of-life improvements emerge through simple but profound connections—like parents of children with the same rare condition finally meeting through network-facilitated support groups. These psychosocial dimensions remind us that effective healthcare transcends laboratory results and treatment protocols.
Looking ahead, the next frontier involves predictive network capabilities. Emerging research into biomarkers and genetic predispositions suggests future networks might identify at-risk individuals before symptom onset. This proactive paradigm would represent a quantum leap from current reactive models. However, it raises ethical questions about genetic privacy and psychological preparedness that networks must address.
The evolution of rare disease networks reflects broader transformations in medicine—from isolated interventions to connected ecosystems, from treating diseases to supporting whole persons, from national solutions to global cooperation. As these networks mature, they offer templates for addressing other complex health challenges where collaboration outperforms fragmentation. Their greatest legacy may ultimately lie in proving that no disease is too rare to deserve attention, and no patient too isolated to receive care.
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025